Diabetic Retinopathy Treatments in Norfolk and Virginia Beach
In diabetic retinopathy the blood vessels of the retina become abnormal and develop tiny leaks, causing fluid or blood to seep into the retina, especially the macula. When fluid accumulates in the macula, it becomes wet and swollen and cannot work properly. This is called macular edema, which causes the central vision to become blurry. The form of diabetic retinopathy caused by leakage of retinal blood vessels is called nonproliferative diabetic retinopathy (NPDR).
Another problem with retinal blood vessels in diabetes is that they can become blocked. If the retinal tissue no longer receives nutrition from the retinal blood vessels, it will stop working properly. The areas of the retina with obstructed blood vessels will foster the growth of abnormal new blood vessels, a process called neovascularization. Neovascularization can cause bleeding and scar tissue that may result in severe loss of vision, or even blindness. The form of diabetic retinopathy in which neovascularization develops is called proliferative diabetic retinopathy (PDR).
Both forms of the eye condition can occur together in an eye.
Symptoms of Diabetic Retinopathy
Though vision may gradually become blurred, significant loss of sight does not usually occur with non-proliferative retinopathy. Since the patient does not experience pain or external symptoms such as bloodshot eyes or discharge, changes in the retina can go unnoticed unless detected by an eye exam.
When bleeding occurs in proliferative retinopathy, the patient has clouding or complete loss of sight. Connective tissue pulling on the retina causes distortion and blurring. However, if abnormalities occur in the peripheral retina, the patient may not experience any symptoms.
Types of Diabetic Retinopathy
Nonproliferative Diabetic Retinopathy (NPDR)
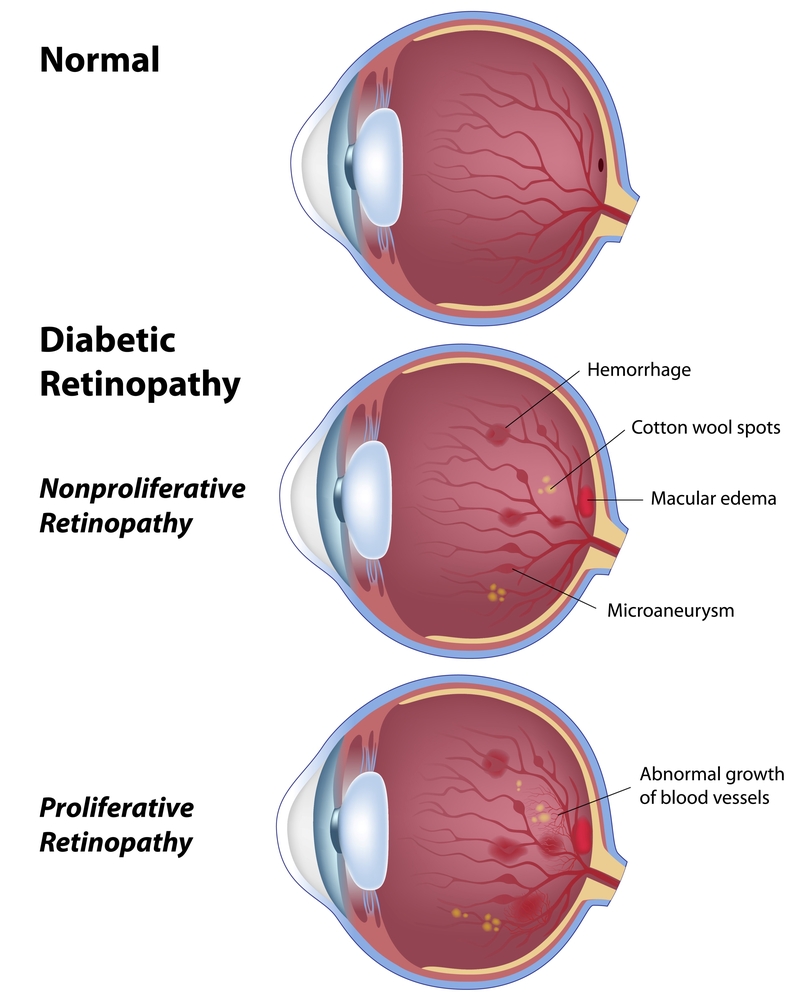
In diabetes, the retinal blood vessels can become damaged and develop tiny leaks. This is called nonproliferative diabetic retinopathy (NPDR). Blood and fluid seem from the tiny leaks, and fatty material (called exudates) can deposit on the retina, causing swelling of the retina. When this swelling occurs on the central part of the retina (the macula), it is called macular edema and vision will be reduced or blurred.
A person with macular edema will usually experience some loss of vision. If one eye is affected, the other eye is also frequently affected. And if each macula is severely disturbed, central vision may be lost from each eye.
Even if the ability to see detail has been lost from both eyes, a person with severe NPDR can usually learn to use areas just outside the macula to see some detail and perform everyday tasks.
Early detection is a person’s best chance of saving their eyesight with laser surgery. Once the macula has been damaged, laser surgery is generally not helpful. For this reason, people with diabetes should test the vision of each eye, every day. One way to test vision is with the Amsler Grid.
Amsler Grid:
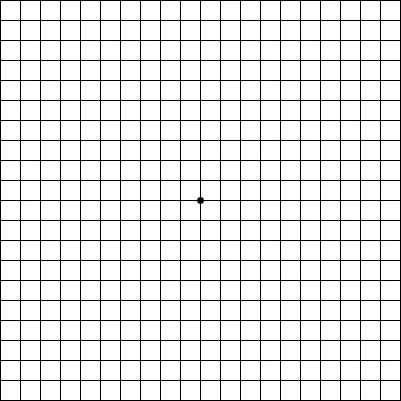
Instructions on using the Amsler grid:
- Wear your reading glasses.
- Cover one eye.
- Look at the center dot and keep your eye focused on it at all times.
- While looking directly at the center, and only the center, be sure that all the lines are straight and all the small squares are the same size.
- If you should notice any area on the grid that becomes distorted, blurred, or discolored, call Virginia Eye Consultants right away.
- Do this test for each eye separately.
Proliferative Diabetic Retinopathy (PDR)
In PDR, large areas of the retinal blood vessels become obstructed causing the retina to lose its source of nutrients. When this happens, peripheral vision is often reduced and the person’s ability to see at night or adjust their site to changes in lighting is often diminished.
The retina will develop new, abnormal blood vessels in an attempt to compensate for its loss of nourishment. This is called neovascularization, and it is very dangerous to the eye. Neovascularization does not nourish the retina properly, and may cause other problems such as bleeding into the vitreous cavity (called vitreous hemorrhage) or the growth of scar tissue on the retina, which can pull the retina off the back wall of the eye (called traction retinal detachment). Either of these severe problems, vitreous hemorrhage or traction retinal detachment, can lead to severe loss of vision or total blindness.
Diabetic Retinopathy Treatment
Treatment for Nonproliferative Diabetic Retinopathy
Laser Surgery
Laser Surgery is used to stop abnormal retinal blood vessels from leaking fluid into the retina, especially the macula. Laser surgery infrequently results in improved vision, but often reduces the loss of further vision.
There are two types of laser surgery for NPDR:
- Focal Laser Surgery treats the leaking spots in the retina with laser photocoagularion in an attempt to stop the leakage. In some cases, the leaks are found by an angiogram, which is then used as a guide for the accurate placement of the laser.
- Grid Laser Surgery is used when retinal blood vessels appear to be leaking everywhere in the macula, not just in a few specific areas. The laser is placed in a grid pattern across the entire swollen macular area.
Even when laser surgery has successfully sealed the leaking vessels, new areas of leakage frequently appear later and must be treated. Patients should continue to check the vision in each eye daily and notify their doctor if there are any new changes.
Intravitreal Injections
Intravitreal injections are also a way to treat nonproliferative diabetic retinopathy. Special drugs are injected into the eye to help slow down vision loss and in some cases improve sight.
- Lucentis is a drug that causes shrinkage of the abnormal blood vessels when it is injected into the eye. The shots need to be repeated every 1 to 3 months. Lucentis can maintain vision in most patients and improve vision in many patients.
- Kenalog contains the active ingredient triamcinolone, which is a type of medicine known as a corticosteroid. Corticosteroids have many important functions in the body, including control of inflammatory responses, such as the swelling of the retina.
Treatment for Proliferative Diabetic Retinopathy
Laser Surgery
The type of laser surgery done for neovascularization is called panretinal laser photocoagulation (PRP), which uses the laser to destroy all of the damaged areas of the retina where the blood vessels have been obstructed. When those areas are destroyed, the retina is likely to stop developing new blood vessels, and those that are already present tend to become inactive or disappear.
Panretinal laser photocoagulation is placed on the sides of the retina, not in the center. After the surgery, side vision may be slightly diminished. These side areas are partially sacrificed in order to save as much of the central vision as possible and to save the eye itself.
Panretinal laser photocoagulation does not improve vision; but it is the best way to prevent further vision loss.
Vitrectomy Surgery
If there is so much vitreous hemorrhage that laser surgery is not possible, the blood can be removed with an operation called vitrectomy, which removes the blood-filled vitreous gel and replaces it with a gas bubble or fluid that is compatible with the eye.
Convenient Locations in and around Norfolk or Virginia Beach. We Look Forward to Seeing You!

200 Corporate Blvd,
Norfolk VA, 23502

2234 Cunningham Dr,
Hampton VA, 23666

241 Corporate Blvd,
Norfolk VA, 23502

241 Corporate Blvd,
Norfolk VA, 23502

2463 Pruden Blvd,
Suffolk VA, 23434

2020 General Booth Blvd,
Virginia Beach VA, 23454

465 N Great Neck Rd,
Virginia Beach VA, 23454
Learn More Today
We invite you to call and learn more about our procedures for treating diabetic retinopathy. Contact us to schedule your consultation with one of our ophthalmologists and learn about your treatment options.
The doctors at Virginia Eye Consultants have either authored or reviewed the content on this site.